Peroneal Tendon Surgery
Peroneal Tendon Surgery Information Sheet
What is Peroneal Tendon Surgery?
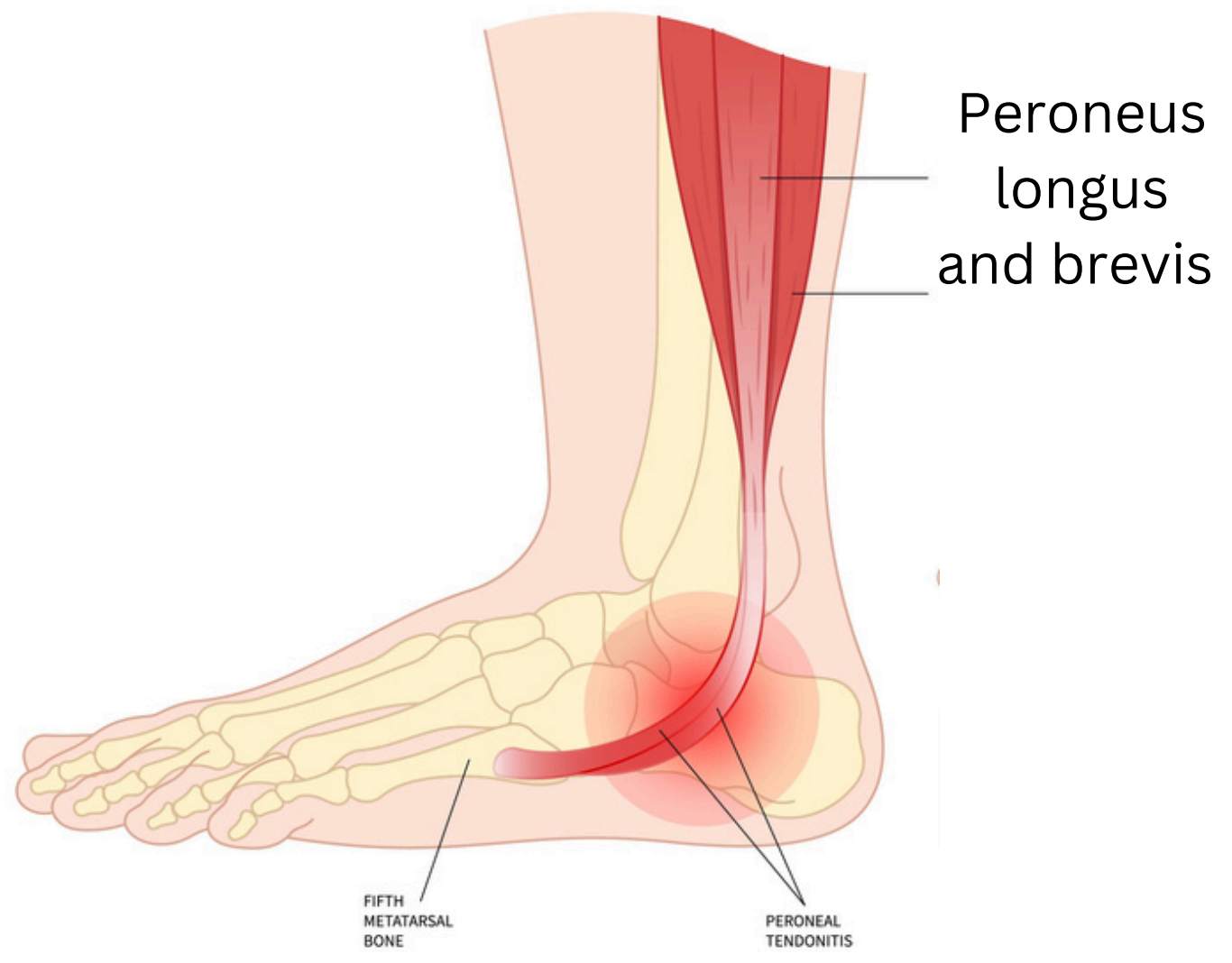
Peroneal tendon surgery is performed to repair or stabilise the peroneal tendons, which run along the outer side of the ankle. These tendons help stabilise the foot and ankle and assist in activities such as walking, running, and balancing on uneven surfaces. Surgery is often required when the tendons are torn, inflamed, unstable, or damaged due to chronic overuse, ankle sprains, or degenerative changes. In such cases, treatment is typically carried out by an experienced Orthopaedic Surgeon in Adelaide to restore strength, reduce pain, and prevent further instability.
Injury to these tendons can cause ongoing pain, weakness, ankle instability, and difficulty with physical activity. When non-surgical treatments like physiotherapy, orthotics, or medications are unsuccessful, surgery becomes a viable option to restore function.
Who is Suitable for Peroneal Tendon Surgery?
Surgery is typically recommended for patients who meet one or more of the following conditions:
- Chronic pain and swelling on the outside of the ankle that does not improve with rest or physiotherapy.
- Partial or complete tears of the peroneal tendons confirmed via imaging (MRI or ultrasound).
- Peroneal tendon subluxation or dislocation, where the tendons slip out of their normal groove.
- Ankle instability associated with high-arched feet (cavus foot) or recurrent ankle sprains.
- Athletes or active individuals who need to regain full ankle strength and mobility for performance.
- Failure of conservative treatments like bracing, or rehabilitation exercises.
Benefits of Peroneal Tendon Surgery
The primary goal of surgery is to restore function and relieve pain. The benefits include:
- Reduced ankle pain and inflammation, particularly during weight-bearing activities.
- Improved ankle stability, which lowers the risk of future sprains or falls.
- Restored tendon function, allowing better foot movement and athletic performance.
- Corrected alignment of the tendons to prevent ongoing dislocation or subluxation.
- Improved quality of life, with the ability to return to walking, running, or sports with confidence.
- Prevention of worsening symptoms or complete rupture
Types of Peroneal Tendon Surgery
There are several surgical techniques depending on the underlying problem:
- Tendon Repair: Tears or splits in the tendons are stitched back together. This is the most common procedure for partial tendon damage.
- Tendon Debridement: Damaged, inflamed, or scarred portions of the tendon are removed, leaving healthy tissue behind.
- Tendon Transfer: In severe cases, the damaged peroneal tendon is replaced or reinforced using another tendon in the foot.
- Groove Deepening (Fibular Groove Deepening): The bony channel that houses the tendons is surgically deepened to prevent tendon dislocation.
- Tendon Stabilisation with Retinaculum Repair: The retinaculum (a ligament that holds the tendons in place) is repaired or reinforced to stop the tendons from snapping over the bone.
- Combined Surgery: Sometimes combined with other procedures like lateral ankle ligament reconstruction or cavovarus foot correction.
Alternative Options to Peroneal Tendon Surgery
Surgery is typically considered when non-surgical treatments have not worked. These conservative options may be recommended first:
- Rest and Activity Modification: Reducing activities that strain the tendons (like running or jumping) to allow healing.
- Immobilisation: Using a boot or brace prevents movement and supports the tendon while it heals.
- Physiotherapy: Strengthening surrounding muscles and improving ankle stability through targeted exercises.
- Anti-inflammatory Medications: NSAIDs such as ibuprofen to reduce swelling and pain.
- Orthotics: Custom shoe inserts to correct foot mechanics, especially in cases of high-arched feet.
- Corticosteroid Injections: Used cautiously to relieve inflammation around the tendon.
- Platelet-Rich Plasma (PRP): In some cases, PRP injections may promote healing in mild to moderate tendon injuries.
While these methods can be effective in early or moderate cases, surgery may be the best choice for long-standing tendon tears, tendon instability, or severe pain that interferes with daily life.
Preparation Before a Peroneal Tendon Surgery
Preparation plays a key role in achieving the best results from peroneal tendon surgery. Here are important steps you may be asked to follow:
- Attend a Pre-Surgical Consultation: Dr. Graff will review your medical history, examine your ankle, and review any imaging, such as X-rays, ultrasound, or MRI scans. This ensures the correct diagnosis and treatment plan.
- Discuss Your Medications: Some medications, such as blood thinners or anti-inflammatory drugs, may need to be stopped or adjusted before surgery to reduce the risk of bleeding or complications.
- Stop Smoking: If you smoke, stopping several weeks before surgery can improve your healing and reduce the risk of infection.
- Plan for Time Off and Assistance: During the early recovery period, when you will be using crutches or a boot, you may need time off work or help at home.
Peroneal Tendon Surgery Procedure
Surgical options may include:
- Debridement of the tendon if the tear involves less than 50% of the tendon
- Excision of the tear if it is greater than 50% of the tendon and attaching it to the intact tendon
- Stabilisation of the tendon if the tendon is unstable by repairing/reconstructing the tissue that usually keeps it in the groove behind the fibula
- Using a tendon graft if both tendons are severely torn and or degenerate
Associated operations may include:
- Ankle stabilisation (see Ankle Stabilisation Surgery)
- Foot reconstruction for a cavovarus foot (see Cavovarus Foot Reconstruction Surgery)
- Ankle arthroscopy (using a camera to look into the ankle) (see Ankle Arthroscopy Surgery)
The Hospital Stay
- You will wake up with a moonboot
- Your foot will be elevated overnight, and you will have antibiotics through a drip.
- You will need blood thinner medication to prevent DVT
- You will stay in the hospital for 1-2 nights
- You will only be allowed to touch your foot to the ground for 2 weeks for balance.
- You will need to take 1g of vitamin C daily.
- Depending on your balance and strength, you may need rehabilitation post-operatively
When You Go Home
- You will need medications for pain relief; regular paracetamol (2 tablets four times a day) is recommended, as well as strong pain killers, especially at night before bed. These can have side effects of drowsiness, nausea and constipation, and other tablets to help with these side effects may be required.
- For six weeks, you will need blood thinners to prevent blood clots and vitamin C for wound healing and pain management.
- You will need a shower chair and bags to keep the moonboot dry for the first 2-3 weeks.
- You will need to attend your post op appointment in 2-3 weeks, where the wounds will be checked.
- After this, you will be able to start seated showering with a shower chair out of the boot.
Peroneal Tendon Surgery Rehabilitation
All patients are different. These timelines are only guides; some patients may progress faster or slower than others.
0 - 3 Weeks
- You will be in a moonboot full time for 2-3 weeks; please treat this like a plaster and do not remove it.
- You will only be allowed to touch your foot to the ground for balance.
- Please keep your foot elevated and out of bed for the toilet only
- You will need to bag the leg for showers
- Pain relief: Please take regular paracetamol with meals and before bed; stronger pain killers are often needed, especially before bed
- Please take blood thinners and vitamin C daily as prescribed
2 - 3 Weeks
- Post op appointment for wound review
- Commence walking in the boot with crutches and increase to full weightbearing without crutches
- Can remove the boot for seated showering but wear it at all other times, including bedtime; be careful not to invert the ankle (move it side to side)
- Start range of motion exercises with physio (dorsiflexion/plantarflexion only)
6 Weeks
- Transition from a boot to a full-time ankle brace and sports shoes (swelling permitting)
- Commence active and passive range of ankle movement, including inversion and eversion, with physiotherapy.
- Commence cycling on an exercise bike
- Static/closed chain peroneal strengthening only
3 Months
- Increase strengthening without restrictions; can start swimming and cycling
- Ease back into sport. Start with jogging, then running, then training
- Once your ankle feels as strong as the other ankle, you can return to sport (also guided by your physio)
6-9 Months
- Full recovery is expected at 9-12 months postoperatively
When can I drive?
- Left foot 2 weeks (if driving an automatic)
- Right foot 6-8 weeks
When can I return to work?
- Seated work at 6-8 weeks
- Prolonged standing 3-4 months
- Heavy labour work 6-9 months in supportive lace-up boots
Peroneal Tendon Surgery Prognosis
Most patients experience significant improvement in pain, stability, and mobility after peroneal tendon surgery. The success rate is high, especially when the tendon is repaired before severe damage or chronic instability develops.
- Positive Outcomes:
- Relief from chronic ankle pain.
- Improved ankle stability and reduced risk of re-injury.
- Return to normal activities and sports for most patients.
- Prevention of further deterioration
- Timeframe:
- Full recovery may take 6- 12 months, but most patients notice steady improvement each month after surgery.
Staying consistent with post-surgical care and physiotherapy greatly improves the chance of long-term success.
Peroneal Tendon Surgery Risks
- Anaesthetic problems
- Nerve injury
- Blood clots
- Infection
- Stiffness
- Ongoing pain or instability
- Arthritis in the ankle joint
- The need for further surgery
What if Peroneal Tendon Surgery is Delayed?
Delaying surgery can have several effects, depending on the severity of your tendon problem:
- Worsening of Tendon Damage: Small tears can progress to complete ruptures or lead to tendon degeneration if left untreated.
- Increased Ankle Instability: Ongoing tendon dysfunction can cause the ankle to give way more easily, leading to more frequent sprains or falls.
- Chronic Pain and Swelling: Unresolved inflammation may continue to limit your activity and affect your quality of life.
- Secondary Problems: Over time, untreated tendon issues can affect other parts of the foot and ankle, leading to changes in walking patterns or additional joint strain.
- More Complex Surgery: The longer the tendon damage is left untreated, the more extensive the surgical repair might need to be.
If your symptoms are significantly affecting your lifestyle and conservative treatments have not helped, it is worth discussing the timing of surgery with your specialist to prevent further complications.
Contact Us
If you want more information or have any questions or problems, please contact Dr Graff at
admin@christygraff.com or call the rooms at
0493 461 133.

