Plantar Fasciitis and Heel Pain
Plantar Fasciitis and Heel Pain Information Sheet
What is Plantar Fasciitis?
Plantar fasciitis is inflammation of the plantar fascia, a thick band of tissue that lies at the bottom of the foot. The plantar fascia runs from the heel bone to the toes, helping to support the arch of your foot.
Plantar fasciitis is one of the most common causes of heel pain. This pain can make it difficult to stand, walk, or run, impacting your mobility and quality of life. For persistent or severe cases, treatment from an experienced Orthopaedic Surgeon in Adelaide can provide effective solutions to relieve pain and restore function.
The plantar fascia works like a shock absorber and supports the arch of the foot during walking and running. When this tissue becomes degenerate, strained or inflamed:
- Foot Mechanics: The arch support weakens, leading to stress on the heel and mid-foot.
- Gait Problems: Pain may cause limping, especially with bare feet on hard surfaces
- Quality of Life: Ongoing pain can make prolonged standing, walking, exercising, or even daily activities uncomfortable, affecting mobility and overall well-being.
Risk Factors for Plantar Fasciitis
Certain groups of people are more likely to develop this condition:
- Age: Most common between 40 and 60 years old.
- Workers on Their Feet: Teachers, nurses, factory workers, or anyone standing for long hours.
- Foot Structure: High arches or a tight Achilles tendon can cause stretch on the plantar fascia
- Lifestyle Factors: Obesity, sudden increase in activity, or wearing poor footwear.
Causes of Plantar Fasciitis
As we age, the tissues in our body lose hydration and degenerate. The plantar fascia functions as a shock absorber and supports the arch of your foot. Excessive pressure over the fascia can strain and tear the tissue, leading to heel pain. When the plantar fascia is repeatedly stretched or stressed, small tears can develop in the tissue, leading to inflammation and pain.
Some common causes of plantar fasciitis include:
- Activities that involve repetitive movements, such as running or jumping, can put excessive stress on the plantar fascia and lead to injury.
- Abnormal foot mechanics, such as high arches or a tight Achilles tendon, can lead to uneven weight distribution on the foot and contribute to the development of plantar fasciitis.
- Excess body weight increases the load on the plantar fascia and contributes to the development of plantar fasciitis.
- Wearing improper shoes that do not provide proper arch support or cushioning can strain the plantar fascia.
- Standing or walking on hard floors for long periods can overwork the plantar fascia.
- As we age, the plantar fascia can become less elastic and more susceptible to injury.
Symptoms of Plantar Fasciitis
The primary symptom of plantar fasciitis is pain in the heel and arch of the foot, which is often worse in the morning (particularly the first few steps of the day), when not wearing shoes or standing/walking on hard surfaces.
Other common symptoms include:
- Stabbing or sharp pain in the heel or arch of the foot.
- Pain that is worse when first standing up or after sitting for some time.
- Pain that decreases after walking or stretching but returns after periods of rest.
- Tenderness or soreness in the heel or arch of the foot.
- Swelling in the affected area.
Prevention of Plantar Fasciitis
Prevention focuses on reducing stress on the plantar fascia and supporting foot health:
- Wear Supportive Footwear: Shoes with good cushioning and arch support.
- Stretch Regularly: Stretch calves, Achilles tendon, and plantar fascia before and after activity.
- Maintain a Healthy Weight: This helps reduce extra stress on the feet.
- Gradual Activity Increases: Avoid sudden increases in exercise or standing time.
- Use Orthotics if Needed: Custom or over-the-counter inserts can provide support for your arches.
Stages of Plantar Fasciitis
Plantar fasciitis often progresses gradually:
- Stage 1 – Early/Mild: Occasional heel or arch pain, often in the morning or after prolonged standing. Symptoms ease with movement.
- Stage 2 – Moderate: Pain becomes more frequent, with tenderness in the heel and arch. Activities like walking, running, or climbing stairs may worsen pain.
- Stage 3 – Severe/Chronic: Persistent pain even at rest. The fascia may thicken, and gait changes can lead to pain in the knees, hips, or back.
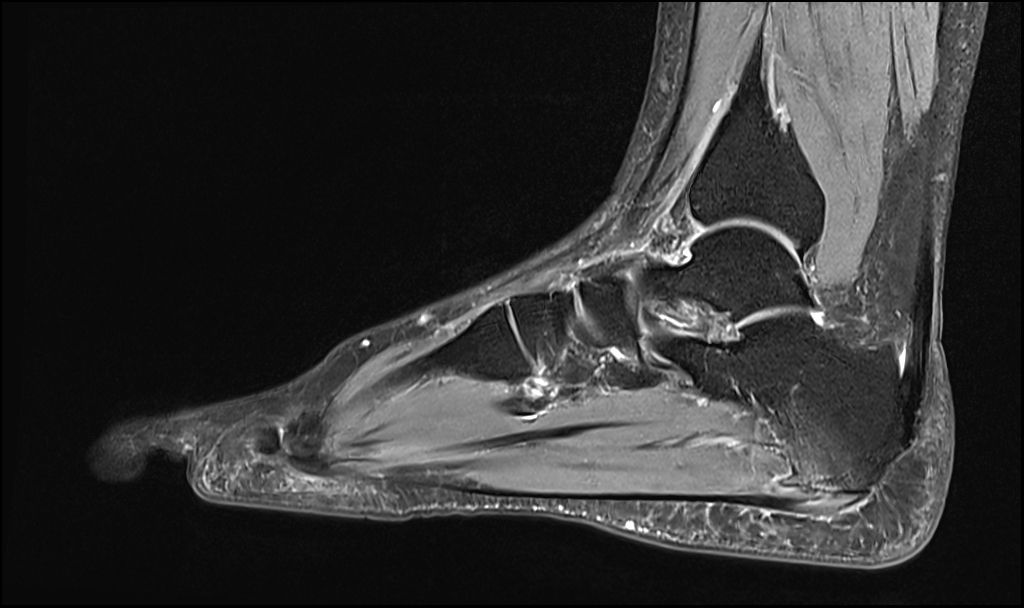
Diagnosis of Plantar Fasciitis
Dr Graff will take a medical and functional history and examine your foot, which includes checking for the signs of flat feet or high arches, tenderness, swelling, redness, stiffness or calf/Achilles tightness.
An X-ray and/or MRI scan may be required. Treatment of Plantar Fasciitis
- Physiotherapy: Stretching your plantar fascia and Achilles tendon strengthens the lower leg and intrinsic foot muscles.
- Podiatry: Podiatrists use techniques such as shockwave therapy, dry needling, laser therapy, and orthotics. Shockwave Therapy involves high-energy acoustic sound waves (shockwaves) being applied to the plantar fascia, which acts through several mechanisms to stimulate a healing response.
- Supportive Shoes and Orthotics: Shoes with appropriate support and cushioning are essential to managing the symptoms of plantar fasciitis. Custom orthotics may also help support the plantar fascia and provide shock absorption and proper load distribution.
- Rest and ice: Decrease or avoid activities that worsen the pain, and icing can help alleviate severe inflammation.
- Medications: Non-steroidal anti-inflammatory drugs (NSAIDs) may be used to reduce pain and inflammation, and should be taken with food.
- Corticosteroid Injection: A steroid (ie cortisone) injection may be indicated, and can also be used as a diagnostic tool
- Surgery: Occasionally, orthopaedic surgery to release the tight plantar fascia may be necessary if conservative measures are ineffective.

